What is Long COVID?
Prof Mark Taylor, MD; FRCPsych; FRCPE; FRANZCP; Kirsty Taylor, BA (Hons); PGCE; FRSA; and
Prof Alan J Carson, FRCPsych; FRCPE
Introduction
In 2019 reports started emanating from Wuhan in China about a novel viral infection, initially thought to be similar to SARS. By March 2020 the world was in the grip of the highly contagious coronavirus COVID-19 pandemic (here referred to as COVID), leading to a series of urban and travel lockdowns across the globe.
Society then completely changed, with people working from home becoming the new norm, and virtually everyone accepting government strictures about mask-wearing; staying in the house most of the day; not seeing sick or elderly relatives, and even avoiding parties (well, politicians were apparently exempt), weddings, and funerals.
By 2021 there were over 2.5 million deaths across 215 countries due to COVID1. Importantly, people with serious mental illness such as schizophrenia and bipolar were found to be at a higher risk of death due to COVID, regardless of smoking status or co-morbidity, reflecting barriers to care and possible immunological disturbance1.
The clinical presentations of COVID were protean, reflecting a multi-system inflammatory response to the virus, usually affecting the lungs, heart, blood vessels and of course the central nervous system. 15% of folk with acute COVID infection required hospitalisation, with 5% of those becoming critically ill2.
Here we review the extant knowledge and reviews of ‘long COVID’ with a particular focus on the persistent neuropsychiatric symptoms after a COVID infection.
What are the ‘long’ term clinical sequelae of COVID?
One of the problems is that the name ‘long COVID’ entered the lexicon from patient groups before any disorder had been defined. Clinical advisory organisations such as NICE, CDC and other authorities have been left trying to fit definitions around the name. Somewhat arbitrarily this is usually taken as suffering from any ongoing symptoms 3 months after acute infection.
In the UK it is thought about 1 in 10 cases post COVID have persistent symptoms2, but estimates vary depending on how one defines a case. So, for instance an isolated ongoing absence of smell may be classed alongside crippling fatigue.
Long COVID has a different clinical constellation to acute COVID, with acute COVID most frequently presenting2 with the following symptoms:
| Fever | 83% |
| Cough | 58% |
| Fatigue | 38% |
| Difficulty breathing | 35% |
| Gut issues | 15% |
| Headache | 6% |
The most common chronic or long COVID symptoms have been reviewed as follows:2,3
| Weakness | 41% |
| Reduced quality of life | 37% |
| General malaise | 33% |
| Fatigue | 31% |
| Poor concentration | 26% |
| Difficulty breathing | 25% |
Many of these common symptoms are largely subjective.
Further analysis in this review3 revealed that women with long COVID had more headache and more smell / taste disturbance than men, and those people who had required intensive care had more long-term muscle pain (myalgia).
Long COVID is clearly a heterogenous condition and possibly comprises several different syndromes. The fears are of organ damage; post-intensive care syndrome and persistent cardio-respiratory problems but to date objective evidence for such conditions has been confined to a small minority.
This may be because the tests are simply not sensitive to detect the pathologies, as has been suggested with theories such as microscopic bloodclots. Others are more sceptical and think that much of what is detected are simply normal variants, and that for the majority the mechanisms may share more in common with chronic fatigue syndromes and functional somatic syndromes.
Risk factors for long COVID
Whilst male gender, medical comorbidities, and older age increase the risk of a more severe acute COVID, that appears not to be the case with long COVID.
Although the data are less robust4 than in acute COVID, the Office of National Statistics in the UK reported long COVID is more common in women than men (24% v 21%), and 53% of all long COVID cases are aged 35-69 years but only 18% are 70 years or over.
Male gender and medical problems such as diabetes; heart disease; and obesity were not associated with long COVID, although a history of asthma was.
Neuropsychiatry of long COVID
For those of us working in mental health and neuropsychiatry, long COVID may well be an increasing focus or concern in the future. Here we examine the neuropsychiatry of long COVID.
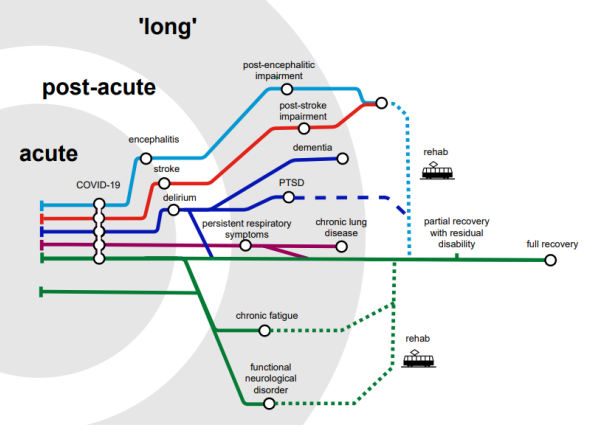
Acute COVID can is associated with delirium/encephalopathy, stroke and more rarely encephalitis. Contrary to early fears it has become clear that the virus rarely infects the brain, but any associated inflammatory ‘cytokine storm’ and hypercoagulation are potential mechanisms of concern.
Taquet and colleagues6 from Oxford showed that in the 6 months after acute COVID infection, about a third of all individuals (n= 236,379) had a neuropsychiatric disorder (incidence 34%, for any diagnosis; 13% for a first diagnosis), which they found (in this large database study) was substantially higher than the rates of these conditions after an comparative influenza infection (n= 105,579 people).
COVID has been associated2 with ischaemic stroke, but Taquet et al also found a later risk of increased dementia (hazard ratio or HR = 1.88). The risks for these disorders seemed to be particularly associated with having delirium and / or an encephalopathy. Of note is that delirium is generally recognised to be associated with a stepwise progression to later neurodegenerative illness. What may be different about COVID is not so much that this happens but that a greater number of patients seem to suffer an acute delirium.
In the same study, the long COVID rates of developing mood disorder (HR = 1.53); anxiety (HR =1.49); substance misuse (HR = 1.68); and insomnia (HR = 1.49) were all elevated but these increased risks were not linked to hospitalisation for COVID, suggesting that perhaps it is the more general psychosocial effects of the pandemic that play a part.
Badenoch et al recently meta-analysed 51 studies looking at the neuropsychiatry of long COVID5. A summary graphic of their findings is given below:
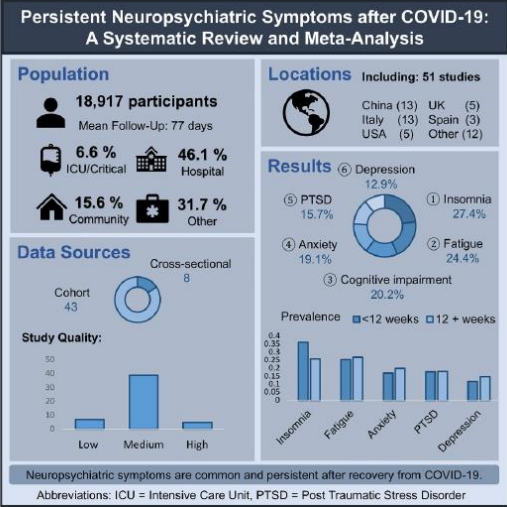
So, it seems long COVID is not the same as but not dissimilar to ‘chronic fatigue syndrome’ (CFS – again, a controversial diagnosis). Which isn’t surprising for a post-viral syndrome. The neuropsychiatric triad of insomnia; fatigue; and cognitive impairment are superimposed onto high rates of depression, anxiety,
and trauma.
Reviews4 suggest ‘brain fog’; fatigue; sleep disturbances; and depression / anxiety / post-traumatic stress / obsessionality are commonly seen in the postacute phase. Some of the former may be related to the need for acute care or ICU, whereas the latter could be secondary to quarantine, isolation, loneliness and social distancing.
Interestingly, first episode psychosis (FEP) in long COVID was more common in those hospitalised for COVID, especially if there was an acute encephalopathy, suggesting that FEP behaves as much like a ‘neurological’ as a ‘psychiatric’ condition. There were caveats to this psychosis data however, for example that the average study age was 53 and the delirium of COVID may have been misunderstood as psychosis.
The multiple pathways to neuropsychiatric disorder post-COVID in the acute; post-acute; and chronic or ‘long COVID’ phases are illustrated in this graphic:
Treatment options
Whilst clinical guidelines, eg from NICE, acknowledge that long COVID exists and should be treated, few specific recommendations are made, reflecting the absence of any evidence base. For example, the advice about breathing problems is to avoid smoking and pollutants and to try a steroid inhaler.
Absent evidence of specific long covid treatments (which may never come to pass) should not deter clinicians as our experience is that a detailed history of the various components of a long covid symptom complex in an individual patient can often give rise to direct treatment targets. For example, the patients may have migrainous headaches, persistent postural perceptual dizziness, brain fog and agoraphobic anxiety – each of which has a recognised and efficacious treatment. There is no reason to suspect the treatment of migraine will change simply because the trigger was COVID, but there is a risk that such therapeutic care may not be offered in favour of the search for a global panacea.
One important area that will need further clinical trials is to assess treatments for fatigue. Unfortunately, we have noted unhelpfully strident tones entering this debate, akin to those in ME/CFS. It is generally unhelpful to push patients into treatment that they are not willing to engage with, but for those who do wish a rehabilitative approach it is worth noting that in all the studies of graded exercise therapy and cognitive behavioural therapy for fatigue no excess of harm has been shown in the treatment arms, nor has the presence or absence of post-exertional malaise had any impact on the likelihood of this.
Furthermore, whilst no specific anti-inflammatory or anti-viral medication has been tested in long COVID, clinical acumen might suggest that activating antidepressants such as fluoxetine or vortioxetine; stimulants like modafinil; and ADHD and anti-dementia treatments may all have a role to play in the pharmacotherapy of long COVID, whilst we wait for definitive trials.
Lastly, bearing in mind the imperative of ‘first do no harm’, a consideration of relatively safe over-the-counter remedies with CNS effects such as probiotics; and antioxidants such as melatonin; vitamins B, C, D and E, and the flavonoid luteolin as well as other polyphenols may well be both acceptable to the patient and worth employing clinically.
Conclusions
Everyone has now heard of ‘long COVID’ but it’s definition and aetiology are elusive. The clinical presentations are varied and often subjective in nature but are similar to other post-viral states, and include fatigue, weakness, and cognitive issues, along with respiratory problems.
The rates of all long COVID neuropsychiatric disorder seem to go up following severe acute COVID associated with encephalopathy, but a causal relationship is less clear when no encephalopathy has occurred.
Increased rates of anxiety and depression with, interestingly, post-traumatic stress, are apparent with long COVID but may in part reflect the non-specific general ramifications of the pandemic such as isolation and loneliness, as well as specific post-viral consequences. These non-specific pandemic effects appear to be more pronounced7 in the younger age (16-25 years) groups.
Clearly, we need more data and understanding on ‘what is long COVID?’ and what we clinicians can do about it.
Professor Mark Taylor, BSc (Hons); MBBS; MD; FRCPsych; FRCP; FRANZCP
References
- Ford G, Nemai K, Etchart D et al. Association between mental health disorders and
mortality among patients with COVID-19 in 7 countries. JAMA Psychiatry (2021) 78
(11) 1208-1217. - Hatmi ZN. A systematic review of systematic reviews on the COVID-19 pandemic. SN
Comprehensive Medicine (2021) 3:419-436 - Michelen M, Manoharan L, Elkheir N et al. Characterising long COVID: a living
systematic review. BMJ Global Health (2021) doi:10, 1136/bmjgh-2021-005427 - Crook H, Raza S, Nowell J et al. Long COVID – mechanisms, risk factors, and
management. BMJ 2021;374:n1648 http://dx.doi.org/10.1136/bmj.n1648 - Badenoch JB, Rengsamy ER, Watson C et al. Persistent neuropsychiatric symptoms
after COVID-19: a systematic review and meta-analysis. Brain Communications (Dec
2021) doi:10.1093/braincomms/fcab297 - Taquet M, Geddes JR, Husain M, Luciano S, Harrison PJ. 6-month neurological and
psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study
using electronic health records. Lancet Psychiatry (2021); 8: 416–27. - Pierce M, Hope H, Ford T et al. Mental health before and during the COVID-19
pandemic: results from a longitudinal probability sample survey of the UK
population. Lancet Psychiatry. 2020. 7: 883-92
Acknowledgement: The authors thank Dr Laura McWhirter.




